Gallstones
What are Gallstones?
Gallstones (biliary calculi) are small pebble-like substances that form in the gallbladder.
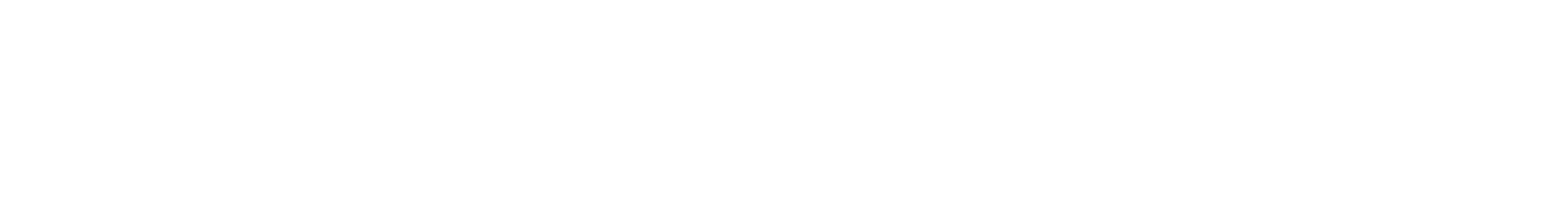
The gallbladder is a small pear-shaped sac that lies below the liver. Bile is made in the liver, and stored in the gallbladder until the body needs it. The presence of fatty foods triggers the gallbladder to squeeze bile into the small intestine. Bile helps with digestion and breaks up dietary fat. It contains water, cholesterol, fats, bile salts, proteins, and bilirubin (a waste product).
If bile contains too much cholesterol, bile salts, or bilirubin, it can harden into gallstones. Gallstones can block the normal flow of
bile if they move from the gallbladder and lodge in any of the ducts that carry bile from the liver to the small intestine.
The ducts include the:
• Hepatic ducts - which carry bile out of the liver.
• Cystic duct - which takes bile to and from the gallbladder
• Common bile duct - which takes bile from the cystic and hepatic duct to the small intestine.
What causes Gallstones?
There is no single cause of gallstones. From the size of a grain of sand to a golf ball. The gallbladder can develop just one large stone, hundreds of tiny stones, or a combination of the two. The three types of gallstones are cholesterol stones, pigment stones and mixed stones. Cholesterol stones If the liver produces too much cholesterol, cholesterol crystals may form in bile and harden to become stones. Cholesterol stones can grow to significant sizes, large enough to block bile ducts. Pigment stones Numerous, small dark stones form because of changes in other bile components or because the gallbladder fails to empty normally. Mixed stones These are the most common type and tend to develop in batches. They are composed of cholesterol and salts.
Gallstones become more common with advancing age and can be found in up to 15% of people 50 years and over. They are more common in women than in men, in people who are overweight and in those with a family history of gallstones. People with diabetes, taking cholesterol lowering medicines or who lose a lot of weight quickly are also more at risk.
What sort of operation might I need?
Treatment will usually require surgery open or laparoscopic removal of stones from the bile duct. If you have frequent gallbladder attacks,
your doctor may recommend you have your gallbladder removed (Cholecystectomy). Surgery to remove the gallbladder, a non-essential organ, is
one of the most common surgeries performed on adults. This surgery is usually done by ‘keyhole’ surgery, using laparoscopes. The operation
requires three small incisions in the abdomen and usually 1 or 2 days in hospital. Occasionally, ‘keyhole’ surgery is impossible or risky
and the gallbladder is instead removed through a longer incision below the right ribs. This is called a laparotomy or open surgery This
requires a longer hospital stay, perhaps up to 8 days.
Operations such as these are very safe but always carry a small risk of problems during surgery (such as bleeding or damage to the bile
duct) and of later complications such as chest infections. Occasionally, x-rays taken during the operation show a stone in the bile
duct that requires a later endoscopic procedure (ERCP as described above).
If you are concerned about possible risks, ask your doctor for further information.
What are the treatment options?
Medical treatment may not be necessary unless the gallstones present symptoms.
Treatment depends on the size and location of the gallstones, but may include:
• Dietary modifications – Limiting or eliminating fatty foods and dairy products.
• Surgery - If you have episodes of pain, your doctor may recommend an operation to remove the stones from the bile duct or the entire
gallbladder, Cholecystectomy
• Lithotripsy - A special machine generates sound waves to shatter stones. This treatment is used for those people with small and soft
stones, which accounts for around two out of 10 cases of gallstones with symptoms.
• Medications-Some drugs can dissolve gallstones but this treatment is only rarely given, due to side effects and a variable success
rate.
Urgent treatment is required if complications such as jaundice or infections in the gallbladder or bile duct occur.
What symptoms do Gallstones cause?
• Pain in the abdomen and back. Pain is generally infrequent but severe.
• Increase in abdominal pain after eating a fatty meal.
Will an operation cure my symptoms?
Surgery will cure many symptoms arising from gallstones.
GORD + HIATUS
What is GORD (GERD)
Gastroesophageal reflux disease (GORD) is defined as the back-flow of stomach contents into the Oesophagus causing undesirable symptoms and potentially resulting in Oesophageal damage.
What is GORD (GERD)
GORD is caused by improper mechanical function of the Lower Oesophageal Sphincter (LOS).
The LOS is a ring of muscle that surrounds the junction of the oesophagus and the stomach and acts as a valve. When functioning properly, this valve opens when swallowing to allow passage of food from the oesophagus into the stomach.
The valve then closes and acts as a barrier to keep stomach contents from refluxing into the oesophagus. In people with GORD, the LOS does not properly close resulting in back-flow of gastric contents. It is the back-flow of gastric contents that cause the symptoms of GORD. In many people, there is no obvious reason for failure of the LOS.
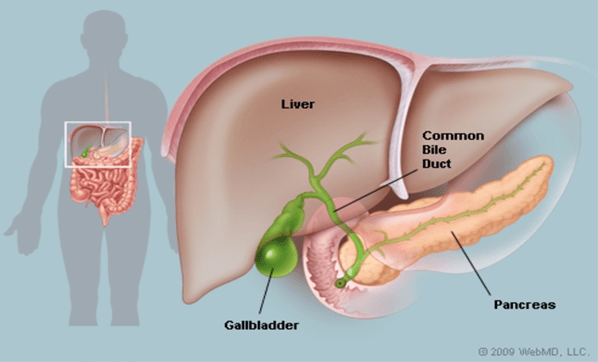
The LOS itself may be weak or its supporting structures (from the oesophagus, the diaphragm, or the angle the oesophagus enters the stomach) may be inadequate. In others, there may be lifestyle or behavioural factors that stress the LOS and contribute to its failure. These factors include: obesity, smoking, alcohol use, a high fat diet, and consumption of carbonated beverages. Additionally, a hiatal hernia can lead to GORD.
Hiatal hernia results when the LOS moves above the diaphragm, a sheet of muscles that separates the abdominal and chest cavities. When the LOS moves into the chest, it is less able to prevent reflux. Finally, GORD symptoms can be compounded by defective clearance of acid and fluid from the lower (distal) oesophagus due to oesophageal damage or oesophageal motility disorders.
Symptoms
The most common symptom of GORD is heartburn. This is an uncomfortable burning sensation felt in the middle of the upper abdomen and/or lower chest. Other typical symptoms include difficulty swallowing (dysphagia) and regurgitation of fluid into the oesophagus. In some cases fluid may even reflux into the mouth.
People with GORD also may develop other, atypical (extraesophageal) symptoms such as hoarseness, throat-clearing, sore throat, wheezing, chronic cough, and even asthma. Many persons suffer from extra-oesophageal reflux symptoms for quite some time before a causal relationship with GORD is established.
This is at least partly related to the fact that there are many other causes for these kinds of symptoms other than GORD.
Antireflux Surgery
Surgery for GORD is known as antireflux surgery and involves a procedure called a fundoplication. The goal of a fundoplication is to reinforce the LOS to recreate the barrier that stops reflux from occurring. This is done by wrapping a portion of the stomach around the bottom of the oesophagus in an effort to strengthen, augment, or recreate the LOS valve. The most common type of fundoplication is a Nissen fundoplication in which the stomach is wrapped 360 degrees around the lower oesophagus. There are also a variety of partial fundoplication techniques. As the name suggests, these techniques involve a wrap which does not go entirely around the oesophagus. The Nissen fundoplication is almost always chosen to control GORD.
Antireflux operations today are most often performed using a minimally invasive surgical technique called laparoscopy. The technique utilizes a narrow tube-like camera and several long, thin operating instruments. In the operating room, the camera and instruments are inserted into the abdomen through several small (less than 1 cm or ½ inch) incisions on the abdominal wall. The operation is then performed within the abdominal cavity using camera magnification. The benefit of this type of minimally invasive technique is that it results in less pain, a shorter hospital stay, a faster return to work, smaller scars, and a lower risk of subsequent wound infections and hernias.
If the surgery cannot be safely completed using laparoscopy, the operation is converted to a traditional open procedure that involves an incision in the upper abdomen. The open technique is both safe and effective, but it sacrifices the aforementioned benefits of laparoscopy.
COLORECTAL SURGERY
COLORECTAL (BOWEL) CANCER
Colorectal cancer is experienced by around 5% of the Australian Population. Colorectal cancer is the unregulated growth in the colon or in the rectum usually starting from a polyp in the bowel.
Bowel cancer, also known as colorectal cancer, can affect any part of the colon or rectum; it may also be referred to as colon cancer or rectal cancer, depending on where the cancer is located.
The colon and rectum are parts of the large intestine. The colon is the longest part of the large intestine (the first 1.8 metres). It receives almost completely digested food from the ceacum (a pouch within the abdominal cavity that is considered to be the beginning of the large intestine), absorbs water and nutrients, and passes waste (stool/faeces/poo) to the rectum.
Causes
There are two kinds of risk factors or causes for bowel cancer – those that can be changed (modifiable) and those that cannot (non-modifiable). Modifiable; Bowel Cancer risk is increased by smoking, being overweight or obese, drinking alcohol, eating processed meats (smoked, cured, salted or preserved) or charred red meat.
These risks can be minimised through diet and lifestyle changes and are referred to as modifiable. Non Modifiable: Age, family history, hereditary conditions and personal health history can also influence bowel cancer risk. These factors cannot be changed. People with certain diseases and illnesses seem to be more prone to developing bowel cancer. These include Type II diabetes, other forms of closely linked cancer such as ovarian or digestive system cancers, and inflammatory bowel diseases (IBD) including Crohn’s and Ulcerative Colitis.
A person’s risk category also depends on how many close relatives have bowel cancer and their age at diagnosis. Someone with several close relatives diagnosed with bowel cancer before age 50 has a much higher risk than someone with no close relatives with bowel cancer. In some family members, bowel cancer develops due to an inherited gene mutation.
Symptoms
During the early stages of bowel cancer, people may have no symptoms, which is why screening is so important. Screening can be done at home is easy and safe. National bowel screening program is a government initiative for people aged between 50-74.
The risk for the individual increases dramatically for the age of 50. If you are outside the ages please consult with your GP if you have concerns.
If you have any of the following symptoms for more than two weeks then it is advisable to see your GP. Blood from your bottom or in
your stools. ( blood in your poo) A change in your bowel habit whether this be persistent or intermittent for no reason (constipation,
diarrhoea or feeling you are not completely emptying your bowels) A change in the appearance of your stools, a change in the shape of
your poo; smaller, narrower or has mucous.
Pain in your abdomen or swelling. Pain in your rectum or anus. Non intentional weight loss, weakness or anaemia.
DIVERTICULAR DISEASE
What is Diverticular Disease? (Sometimes referred to as Diverticulitis) It is quite common, some of us do not know that we have it. Diverticular disease is where we develop pockets or a few pouches in the colon, more commonly in the sigmoid colon.
The disease is more common in older people. Sometimes surgical treatment is not necessary. Other times surgical treatment is the only
solution. Symptoms Diverticulosis can cause symptoms that trouble a patient but few of the notable symptoms are as follows: In case of
Diverticulitis
• Alternating episodes of diarrhoea and constipation
• Painful cramps or tenderness in the lower abdomen
• Chills and/or fever
• Nausea and/or vomiting
• Loss of appetite
• Weight loss In case of Diverticular bleeding
• Red or dark red coloured blood in stools
• Dizziness
• Weakness
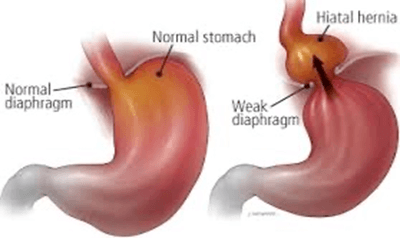
Colectomy
What is a Colectomy
Colectomy is surgery to remove part of the colon that is diseased. This can be performed ‘laparoscopically’ (keyhole surgery)or as an ‘open procedure’ The need for a Colectomy may be from cancer of the colon, inflammatory bowel disease such as Chron’s and ulcerative colitis, blocked bowel, a hole or tear in the bowel wall, repeated diverticulitis, fistula, precancerous polyps.
Types of Colectomy
PERIANAL ABSCESS
What is a perianal abscess?
A perianal abscess can develop where a gland is blocked and causes an infection, pus collects which then forms an enlarged cavity near the anus.
Symptoms
Most common symptom is a lump near the anus along with acute pain in that area. There may also be discharge from that area and can cause pain during your bowel motions. It is not unusual to cause constipation and to have a temperature and to feel generally unwell.
ANAL FISSURES
What is an Anal Fissure?
This is where the linings in your anus tear. Anal Fissures are caused where the texture of your faeces or stools has changed. For example, you have become constipated or even had lose stools over a period of time.
Symptoms
Bleeding from the anus, Severe pain when having a Bowel motion, swelling in the skin on the outside of the anus and a skin tag forming.
PILONIDAL DISEASE
What is Pilonidal disease
Pilonidal means Hair Nest in Latin. This means that hair gets caught in the sinus near the cleft or crease of your bottom and then becomes infected. They form pathways or channels between openings.
Symptoms
Symptoms vary from a small lump, small pit or hole to a large painful and infected abscess. There may be clear or cloudy bloody fluid from the area. Prolonged sitting or certain physical activity may aggravate the area
FISTULA
What is a fistula
This means that an abnormal tunnel has formed between two parts of your body that are not normally joined. For example, an anal fistula is where a connection between the lining of the anus and external skin.
Symptoms
Pain, swelling or discharge of blood or pus from the anus.