GORD + Hiatus
GORD + HIATUS
What is GORD (GERD)
Gastroesophageal reflux disease (GORD) is defined as the back-flow of stomach contents into the Oesophagus causing undesirable symptoms and potentially resulting in Oesophageal damage.
What is GORD (GERD)
GORD is caused by improper mechanical function of the Lower Oesophageal Sphincter (LOS).
The LOS is a ring of muscle that surrounds the junction of the oesophagus and the stomach and acts as a valve. When functioning properly, this valve opens when swallowing to allow passage of food from the oesophagus into the stomach.
The valve then closes and acts as a barrier to keep stomach contents from refluxing into the oesophagus. In people with GORD, the LOS does not properly close resulting in back-flow of gastric contents. It is the back-flow of gastric contents that cause the symptoms of GORD. In many people, there is no obvious reason for failure of the LOS.
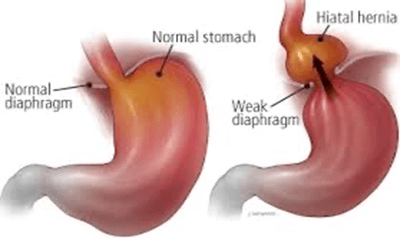
The LOS itself may be weak or its supporting structures (from the oesophagus, the diaphragm, or the angle the oesophagus enters the stomach) may be inadequate. In others, there may be lifestyle or behavioural factors that stress the LOS and contribute to its failure. These factors include: obesity, smoking, alcohol use, a high fat diet, and consumption of carbonated beverages. Additionally, a hiatal hernia can lead to GORD.
Hiatal hernia results when the LOS moves above the diaphragm, a sheet of muscles that separates the abdominal and chest cavities. When the LOS moves into the chest, it is less able to prevent reflux. Finally, GORD symptoms can be compounded by defective clearance of acid and fluid from the lower (distal) oesophagus due to oesophageal damage or oesophageal motility disorders.
Symptoms
The most common symptom of GORD is heartburn. This is an uncomfortable burning sensation felt in the middle of the upper abdomen and/or lower chest. Other typical symptoms include difficulty swallowing (dysphagia) and regurgitation of fluid into the oesophagus. In some cases fluid may even reflux into the mouth.
People with GORD also may develop other, atypical (extraesophageal) symptoms such as hoarseness, throat-clearing, sore throat, wheezing, chronic cough, and even asthma. Many persons suffer from extra-oesophageal reflux symptoms for quite some time before a causal relationship with GORD is established.
This is at least partly related to the fact that there are many other causes for these kinds of symptoms other than GORD.
Antireflux Surgery
Surgery for GORD is known as antireflux surgery and involves a procedure called a fundoplication. The goal of a fundoplication is to reinforce the LOS to recreate the barrier that stops reflux from occurring. This is done by wrapping a portion of the stomach around the bottom of the oesophagus in an effort to strengthen, augment, or recreate the LOS valve. The most common type of fundoplication is a Nissen fundoplication in which the stomach is wrapped 360 degrees around the lower oesophagus. There are also a variety of partial fundoplication techniques. As the name suggests, these techniques involve a wrap which does not go entirely around the oesophagus. The Nissen fundoplication is almost always chosen to control GORD.
Antireflux operations today are most often performed using a minimally invasive surgical technique called laparoscopy. The technique utilizes a narrow tube-like camera and several long, thin operating instruments. In the operating room, the camera and instruments are inserted into the abdomen through several small (less than 1 cm or ½ inch) incisions on the abdominal wall. The operation is then performed within the abdominal cavity using camera magnification. The benefit of this type of minimally invasive technique is that it results in less pain, a shorter hospital stay, a faster return to work, smaller scars, and a lower risk of subsequent wound infections and hernias.
If the surgery cannot be safely completed using laparoscopy, the operation is converted to a traditional open procedure that involves an incision in the upper abdomen. The open technique is both safe and effective, but it sacrifices the aforementioned benefits of laparoscopy.